Product
고객님과의 약속을 소중히 생각합니다.
Product
고객님과의 약속을 소중히 생각합니다.
제품소개
의료정보
병원솔루션
보험심사청구지원
Hospital Solutions
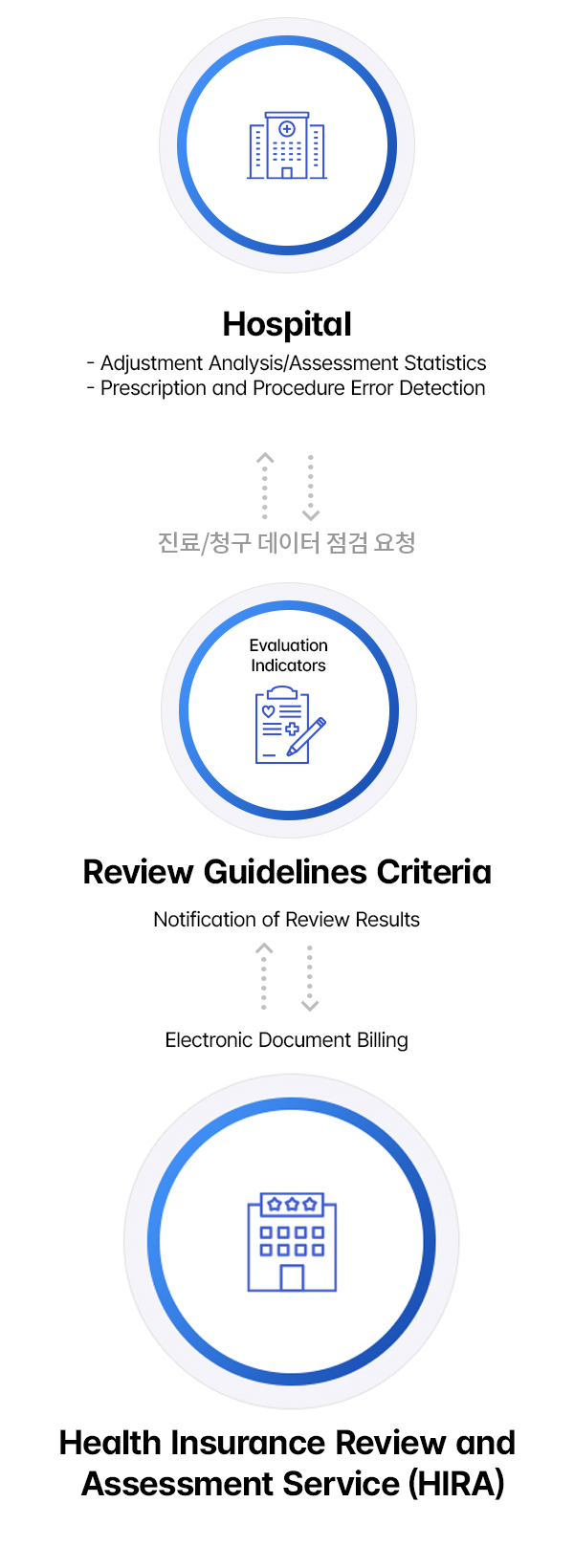
Medigent-Pro is a comprehensive insurance claim support service based on the “Health Insurance Benefit Standards” that has been tested and refined over years of operation in over 250 medium and large hospitals. The service leverages a verified expert database to analyze treatment patterns and billing types, providing pre-claim consultation, post-claim analysis, and efficient decision-making support. Medigent-Pro is designed to help hospitals streamline their insurance claims, improve management practices, and achieve operational innovation.

Medigent-Pro is designed to help hospitals realize their management goals by ensuring
Error Check Based on Standardized Billing Methods:
Prevents data errors and mistakes in claim preparation, blocking rejected submissions and preventing unprocessable claims.
Checks claim codes and data against the latest pricing information, while adapting to changes in regulatory layouts with flexible responses to system updates.
Review of Potential Adjustments Based on Health Insurance Criteria:
Provides information on examination trends and monitors disease linkage to minimize operational mistakes and prevent billing errors.
Prevents claim leakage by ensuring accurate medical fee calculations.
Analysis and Statistics Based on Review Results
Offers diverse and accurate statistical data to enhance hospital management and efficiency.
Identifies medical practice patterns by conducting detailed cost reduction analyses by department and doctor.
Speeds up the process with convenient appeals/reconsideration claim adjustments.
Improved Work Efficiency through Minimizing Manual Work
Reduces error-prone claims caused by human mistakes
Minimizing the Need for Additional Adjustments to Existing Systems
Provides a standardized interface to streamline integration.
Enhances Hospital Image and Trust by Minimizing Error Claims
Builds credibility and improves the hospital’s reputation by reducing errors in claims.
Medigent-Pro utilizes a two-step check process and review result analysis to forecast adjustments in long-term care benefit claims. By providing quick and accurate analysis/statistical information on review decisions, it enhances the efficiency of the review and billing process.
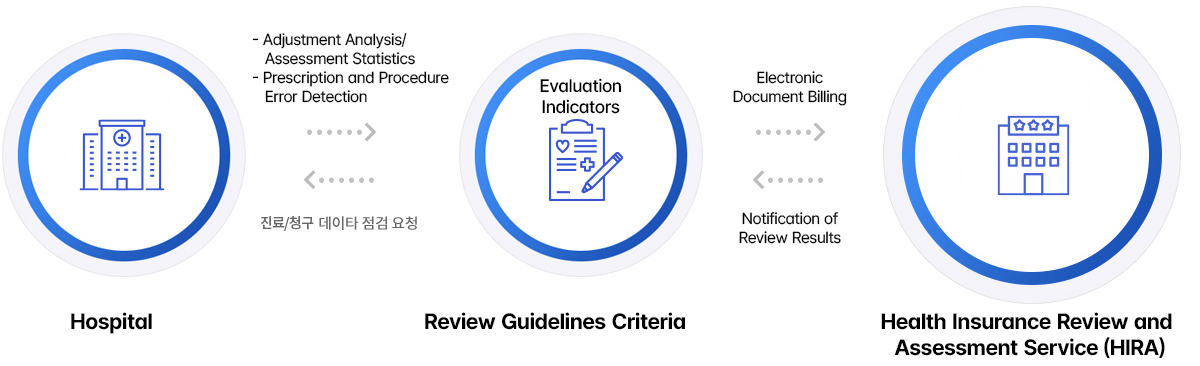
Billing Method Check
Review Adjustment Target Based on Health Insurance Standards
Deduction Analysis and Statistical Management
Improved Management Efficiency
Enhanced Operational Efficiency
Flexible Response to Regulatory Changes
EDI Billing Support
Direct link to the related site.
TOP